9 Personality Disorders
This is an edited and adapted chapter by Crego, C. & Widiger, T. (2019) for the NOBA series in psychology, and an OER textbook by Alexis Bridley and Lee. W. Daffin Jr. For full attribution see end of chapter.
The purpose of this module is to define what is meant by a personality disorder, identify the five domains of general personality (i.e., neuroticism, extraversion, openness, agreeableness, and conscientiousness), identify the six personality disorders proposed for retention in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (i.e., borderline, antisocial, schizotypal, avoidant, obsessive-compulsive, and narcissistic), summarize the etiology for antisocial and borderline personality disorder, and identify the treatment for borderline personality disorder (i.e., dialectical behavior therapy and mentalization therapy).Learning Objectives
- Define what is meant by a personality disorder.
- Identify the five domains of general personality.
- Identify the six personality disorders proposed for retention in DSM-5.
- Summarize the etiology for antisocial and borderline personality disorder.
- Identify the treatment for borderline personality disorder and antisocial personality disorder.
Introduction
Everybody has their own unique personality; that is, their characteristic manner of thinking, feeling, behaving, and relating to others (John, Robins, & Pervin, 2008). Some people are typically introverted, quiet, and withdrawn; whereas others are more extraverted, active, and outgoing. Some individuals are invariably conscientiousness, dutiful, and efficient; whereas others might be characteristically undependable and negligent. Some individuals are consistently anxious, self-conscious, and apprehensive; whereas others are routinely relaxed, self-assured, and unconcerned. Personality traits refer to these characteristic, routine ways of thinking, feeling, and relating to others. There are signs or indicators of these traits in childhood, but they become particularly evident when the person is an adult. Personality traits are integral to each person’s sense of self, as they involve what people value, how they think and feel about things, what they like to do, and, basically, what they are like most every day throughout much of their lives.
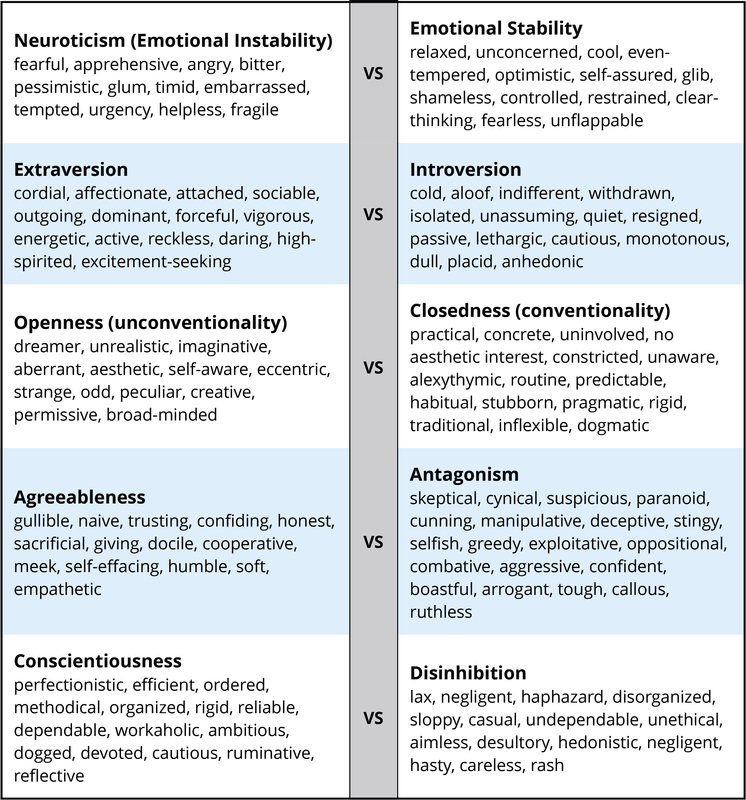
There are literally hundreds of different personality traits. All of these traits can be organized into the broad dimensions referred to as the Five-Factor Model (John, Naumann, & Soto, 2008). These five broad domains are inclusive; there does not appear to be any traits of personality that lie outside of the Five-Factor Model. This even applies to traits that you may use to describe yourself. Table I provides illustrative traits for both poles of the five domains of this model of personality. A number of the traits that you see in this table may describe you. If you can think of some other traits that describe yourself, you should be able to place them somewhere in this table.
DSM-5 Personality Disorders
When personality traits result in significant distress, social impairment, and/or occupational impairment, they are considered to be a personality disorder (American Psychiatric Association, 2013). The authoritative manual for what constitutes a personality disorder is provided by the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM), the current version of which is DSM-5 (APA, 2013). The DSM provides a common language and standard criteria for the classification and diagnosis of mental disorders. This manual is used by clinicians, researchers, health insurance companies, and policymakers. DSM-5 includes 10 personality disorders: antisocial, avoidant, borderline, dependent, histrionic, narcissistic, obsessive-compulsive, paranoid, schizoid, and schizotypal. All 10 of these personality disorders will be included in the next edition of the diagnostic manual, DSM-5. This list of 10 though does not fully cover all of the different ways in which a personality can be maladaptive.
Description
Each of the 10 DSM-5 personality disorders is a constellation of maladaptive personality traits, rather than just one particular personality trait (Lynam & Widiger, 2001). In this regard, personality disorders are “syndromes.” For example, avoidant personality disorder is a pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation (APA, 2013), which is a combination of traits from introversion (e.g., socially withdrawn, passive, and cautious) and neuroticism (e.g., self-consciousness, apprehensiveness, anxiousness, and worrisome). Dependent personality disorder includes submissiveness, clinging behavior, and fears of separation (APA, 2013), for the most part a combination of traits of neuroticism (anxious, uncertain, pessimistic, and helpless) and maladaptive agreeableness (e.g., gullible, guileless, meek, subservient, and self-effacing). Antisocial personality disorder is, for the most part, a combination of traits from antagonism (e.g., dishonest, manipulative, exploitative, callous, and merciless) and low conscientiousness (e.g., irresponsible, immoral, lax, hedonistic, and rash). See the 1967 movie, Bonnie and Clyde, starring Warren Beatty, for a nice portrayal of someone with antisocial personality disorder.
Some of the DSM-5 personality disorders are confined largely to traits within one of the basic domains of personality. For example, obsessive-compulsive personality disorder is largely a disorder of maladaptive conscientiousness, including such traits as workaholism, perfectionism, punctilious, ruminative, and dogged; schizoid personality disorder is confined largely to traits of introversion (e.g., withdrawn, cold, isolated, placid, and anhedonic); borderline personality disorder is largely a disorder of neuroticism, including such traits as emotionally unstable, vulnerable, overwhelmed, rageful, depressive, and self-destructive. Histrionic personality disorder is largely a disorder of maladaptive extraversion, including such traits as attention-seeking, seductiveness, melodramatic emotionality, and strong attachment needs (see the 1951 film adaptation of Tennessee William’s play, Streetcar Named Desire, starring Vivian Leigh, for a nice portrayal of this personality disorder).
It should be noted though that a complete description of each DSM-5 personality disorder would typically include at least some traits from other domains. For example, antisocial personality disorder (or psychopathy) also includes some traits from low neuroticism (e.g., fearlessness and glib charm) and extraversion (e.g., excitement-seeking and assertiveness); borderline includes some traits from antagonism (e.g., manipulative and oppositional) and low conscientiousness (e.g., rash); and histrionic includes some traits from antagonism (e.g., vanity) and low conscientiousness (e.g., impressionistic). Narcissistic personality disorder includes traits from neuroticism (e.g., reactive anger, reactive shame, and need for admiration), extraversion (e.g., exhibitionism and authoritativeness), antagonism (e.g., arrogance, entitlement, and lack of empathy), and conscientiousness (e.g., acclaim-seeking). Schizotypal personality disorder includes traits from neuroticism (e.g., social anxiousness and social discomfort), introversion (e.g., social withdrawal), unconventionality (e.g., odd, eccentric, peculiar, and aberrant ideas), and antagonism (e.g., suspiciousness).
The APA currently conceptualizes personality disorders as qualitatively distinct conditions; distinct from each other and from normal personality functioning. However, included within an appendix to DSM-5 is an alternative view that personality disorders are simply extreme and/or maladaptive variants of normal personality traits, as suggested herein. Nevertheless, many leading personality disorder researchers do not hold this view (e.g., Gunderson, 2010; Hopwood, 2011; Shedler et al., 2010). They suggest that there is something qualitatively unique about persons suffering from a personality disorder, usually understood as a form of pathology in sense of self and interpersonal relatedness that is considered to be distinct from personality traits (APA, 2012; Skodol, 2012). For example, it has been suggested that antisocial personality disorder includes impairments in identity (e.g., egocentrism), self-direction, empathy, and capacity for intimacy, which are said to be different from such traits as arrogance, impulsivity, and callousness (APA, 2012).
Treatment
Personality disorders are relatively unique because they are often “ego-syntonic;” that is, often people with personality disorders are largely comfortable with themselves, with their characteristic manner of behaving, feeling, and relating to others. Ego–syntonic refers to instincts or ideas that are acceptable to the self; that are compatible with one’s values and ways of thinking, even if one’s way of thinking is highly distored. … Ego–dystonic refers to thoughts, impulses, and behaviors that are felt to be repugnant, distressing, unacceptable or inconsistent with one’s self-concept. A person with a personality disorder may not be aware of their personality disorder. As a result of the ego-syntonic nature of personality disorders, people rarely seek treatment for certain types of personality disorders including antisocial, narcissistic, histrionic, paranoid, and/or schizoid personality disorders. People typically lack insight into the maladaptivity of their personality, although eventually people may become aware their personality is dysfunctional through repeated problems in interpersonal interactions, including repeated relationship problems with family and at work. It should be said however that some personality disorders such as those suffering from extreme Borderline Personality Disorder and avoidant personality disorders, are quite aware of their suffering and would like a way to change this.

Those suffering with moderate to severe diagnoses of borderline personality disorder have a tendency to notice difficulties in psychological and interpersonal functioning. Borderline personality disorder relates to high Neuroticism. Neuroticism is the domain of general personality structure that concerns inherent feelings of emotional pain and suffering, including feelings of distress, anxiety, depression, self-consciousness, helplessness, and vulnerability. Persons who have very high elevations on neuroticism (i.e., persons with borderline personality disorder) experience life as one of pain and suffering, and they will seek treatment to alleviate this severe emotional distress. People with avoidant personality may also seek treatment for their high levels of neuroticism (anxiousness and self-consciousness) and introversion (social isolation). In contrast, narcissistic individuals will rarely seek treatment to reduce their arrogance; paranoid persons rarely seek treatment to reduce their feelings of suspiciousness; and antisocial people rarely (or at least willfully) seek treatment to reduce their disposition for criminality, aggression, and irresponsibility.
Maladaptive personality traits will be evident in many individuals seeking treatment for other mental disorders, such as anxiety, mood, or substance use. Many of the people with a substance use disorder will have antisocial personality traits; many of the people with mood disorder will have borderline personality traits. The prevalence of personality disorders within clinical settings is estimated to be well above 50% (Torgersen, 2012). As many as 60% of inpatients within some clinical settings are diagnosed with borderline personality disorder (APA, 2000). Antisocial personality disorder may be diagnosed in as many as 50% of inmates within a correctional setting (Hare et al., 2012). It is estimated that 10% to 15% of the general population meets criteria for at least one of the 10 DSM-IV-TR personality disorders (Torgersen, 2012), and quite a few more individuals are likely to have maladaptive personality traits not covered by one of the 10 DSM-5 diagnoses.
The presence of a personality disorder will often have an impact on the treatment of other mental disorders, typically inhibiting or impairing responsivity. Antisocial persons will tend to be irresponsible and negligent; borderline persons can form intensely manipulative attachments to their therapists; paranoid patients will be unduly suspicious and accusatory; narcissistic patients can be dismissive and denigrating; and dependent patients can become overly attached to and feel helpless without their therapists.
It is a misnomer, though, to suggest that personality disorders cannot themselves be treated. Personality disorders are among the most difficult of disorders to treat because they involve well-established behaviors that can be integral to a client’s self-image (Millon, 2011). Nevertheless, much has been written on the treatment of personality disorder (e.g., Beck, Freeman, Davis, & Associates, 1990; Gunderson & Gabbard, 2000), and there is empirical support for clinically and socially meaningful changes in response to psychosocial and pharmacologic treatments (Perry & Bond, 2000). The development of an ideal or fully healthy personality structure is unlikely to occur through the course of treatment, but given the considerable social, public health, and personal costs associated with some of the personality disorders, such as the antisocial and borderline, even just moderate adjustments in personality functioning can represent quite significant and meaningful change.
Nevertheless, manualized and/or empirically validated treatment protocols have been developed for only one personality disorder, borderline (APA, 2001). This means that there is a well-researched protocol for how to treat issues with borderline personality disorder. There are many theories and types of treatment for other personality disorders, but treatment protocols are not as specific.
Treatment of Borderline Personality Disorder
Dialectical behavior therapy is a form of cognitive-behavior therapy that draws on principles from Zen Buddhism, dialectical philosophy, and behavioral science. The treatment has four components: individual therapy, group skills training, telephone coaching, and a therapist consultation team, and will typically last a full year. As such, it is a relatively expensive form of treatment, but research has indicated that its benefits far outweighs its costs, both financially and socially.
DBT was developed in the late 1980s by Dr. Marsha Linehan and colleagues when they discovered that cognitive behavioral therapy alone did not work as well as expected in patients with borderline personality disorder. Dr. Linehan and her team added techniques and developed a treatment which would meet the unique needs of these patients. DBT is derived from a philosophical process called dialectics.
Dialectics makes three basic assumptions:
- All things are interconnected.
- Change is constant and inevitable.
- Opposites can be balanced and integrated to form a closer approximation of the truth.
Thus in DBT, the patient and therapist are working to resolve the seeming contradiction between self-acceptance and change in order to bring about positive changes in the patient.
Another way to think of DBT is the process of balancing opposites. The therapist consistently works with the individual to find ways to hold two seemingly opposite perspectives at once, promoting balance and avoiding all-or-nothing styles of thinking. In service of this balance, DBT promotes a both-and rather than an either-or outlook. An example of this is if a person feels an emotion such as being angry, there are many actions that they might take to express their angry feelings. But if the action that they take is one that is opposite to the emotion they feel, like walking away from a situation when they are angry, or distracting themselves with something nice or something different, then they have put their energy into something that is eventually going to make them feel better. The way they have done this is to accept and study the emotion of anger, and act in an opposite way to how they have previously believed the emotion directs them to act. This deeper understanding, that a person can have one emotion yet make a opposite or different decision about how to act, grows a general personal awareness that opposites can be balanced and managed in a reasonable way.
Another technique offered by Linehan and her colleagues was validation. Linehan and her team found that with validation, along with the push for change, patients were more likely to cooperate and less likely to suffer distress at the idea of change. The therapist validates that the person’s actions “make sense” within the context of their personal experiences without necessarily agreeing that they are the best approach to solving the problem.
People undergoing DBT are taught how to effectively change their behavior using two skill sets related to acceptance, and two skill sets related to change.
Acceptance skill sets include:
- Mindfulness—focusing on the present (“living in the moment”).
- Distress Tolerance—learning to accept oneself and the current situation. More specifically, people learn how to tolerate or survive crises using these four techniques: distraction, self-soothing, improving the movement, and thinking of pros and cons.
Change skill sets include:
- Interpersonal Effectiveness—how to be assertive in a relationship (for example, expressing needs and saying “no”) but still keeping that relationship positive and healthy.
- Emotion Regulation—recognizing and coping with negative emotions (for example, anger) and reducing one’s emotional vulnerability by increasing positive emotional experiences.
A Dimensional View
A Review of the Ten Personality Disorders
Paranoid personality disorder. Paranoid personality disorder is characterized by a marked distrust or suspicion of others. Individuals interpret and believe that other’s motives and interactions are intended to harm them, and therefore, they are skeptical about establishing close relationships outside of family members—although at times even family members actions are also believed to be malevolent (APA, 2013). Individuals with paranoid personality disorder often feel as though they have been deeply and irreversibly hurt by others even though there lacks evidence to support that others intended to or actually did hurt them. Because of these persistent suspicions, they will doubt relationships that show true loyalty or trustworthiness.
Individuals with paranoid personality disorder are also hesitant to share any personal information or confide in others as they fear the information will be used against them (APA, 2013). Additionally, benign remarks or events are often interpreted as demeaning or threatening. For example, if an individual with paranoid personality disorder was accidently bumped into at the store, they would interpret this action as intentional, with the purpose of causing them injury. Because of this, individuals with paranoid personality disorder are quick to hold grudges and unwilling to forgive insults or injuries- whether intentional or not (APA, 2013). They are known to quickly, and angrily counterattack either verbally or physically in situations where they feel they were insulted.
Schizoid personality disorder. Individuals with schizoid personality disorder display a persistent pattern of avoidance from social relationships along with a limited range of emotion among social relationships (APA, 2013). Similar to those with paranoid personality disorder, individuals with schizoid personality disorder do not have many close relationships; however, unlike paranoid personality disorder, this lack of relationship is not due to suspicious feelings, but rather, the lack of desire to engage with others and the preference to engage in solitary behaviors. Individuals with schizoid personality disorder are often viewed as “loners” and prefer activities where they do not have to engage with others (APA, 2013). Established relationships rarely extends outside that of family as those diagnosed with schizoid personality disorder make no effort to start or maintain friendships. This lack of establishing social relationships also extends to sexual behaviors, as those with schizoid personality disorder report a lack of interest in engaging in sexual experiences with others.
With regard to limited range of emotion, individuals with schizoid personality disorder are often indifferent to criticisms or praises of others and appear to not be affected by what others think of them (APA, 2013). Individuals will rarely show any feelings or expression of emotions and are often described as having a “bland” exterior (APA, 2013). In fact, individuals with schizoid personality disorder rarely reciprocate facial expressions or gestures typically displayed in normal conversations such as smiles or nods. Because of these lack of emotions, there is limited need for attention or acceptance.
Schizotypal personality disorder. Schizotypal personality disorder is characterized by a range of impairment in social and interpersonal relationships due to discomfort in relationships, along with odd cognitive and/or perceptual distortions and eccentric behaviors (APA, 2013). Similar to those with schizoid personality disorder, individuals also seek isolation and have few, if any established relationships outside of family members.
One of the most prominent features of schizotypal personality disorder is ideas of reference, or the belief that unrelated events pertain to them in a particular and unusual way. Ideas of reference also lead to superstitious behaviors or preoccupation with paranormal activities that are not generally accepted in their culture (APA, 2013). The perception of special or magical powers such as the ability to mind read or control other’s thoughts has also been documented in individuals with schizotypal personality disorder. Similar to schizophrenia, unusual perceptual experiences such as auditory hallucinations, as well as unusual speech patterns of derailment or incoherence are also present.
Similar to the other personality disorder within cluster A, there is also a component of paranoia or suspiciousness of other’s motives. Additionally, individuals with schizotypal personality disorder also display inappropriate or restricted affect, thus impacting their ability to appropriately interact with others in a social context. Significant social anxiety is often also present in social situations, particularly in those involving unfamiliar people. The combination of limited affect and social anxiety contributes to their inability to establish and maintain personal relationships; most individuals with schizotypal personality disorder prefer to keep to themselves in efforts to reduce this anxiety.
Antisocial personality disorder. The essential feature of antisocial personality disorder is the persistent pattern of disregard for, and violation of, the rights of others. The pattern of this behavior begins in late childhood or early adolescence and continues throughout adulthood. While the presence of this behavior begins prior to age 15, the individual cannot be diagnosed with antisocial personality disorder until the age of 18. Prior to age 18, the individual would be diagnosed with Conduct Disorder. Although not discussed in this course as it is a disorder of childhood, conduct disorder involves repetitive and persistent pattern of behaviors that violate the rights of others or major age-appropriate norms (APA, 2013). Common behaviors of individuals with conduct disorder that go on to develop antisocial personality disorder are aggression toward people or animals, destruction of property, deceitfulness or theft, or serious violation of rules (APA, 2013).
While commonly referred to as “psychopaths” or “sociopaths,” individuals with antisocial personality disorder fail to conform to social norms. This also includes legal rules as individuals with antisocial personality disorder are often repeatedly arrested for violation of property destruction, harassing/assaulting others, or stealing (APA, 2013). Deceitfulness is another hallmark symptom of antisocial personality disorder as individuals often lie repeatedly, generally as a means to gain profit or pleasure. There is also a pattern of impulsivity- decisions are made in the moment without forethought of personal consequences or consideration for others (Lang et al., 2015). This impulsivity also contributes to their inability to withhold jobs as they are more likely to impulsively quit their jobs (Hengartner et al., 2014). Employment instability, along with impulsivity, also impacts their ability to manage finances; it is not uncommon to see individuals with antisocial personality disorder to large debts that they are unable to pay (Derefinko & Widiger, 2016).
While also likely related to impulsivity, individuals with antisocial personality disorders tend to be extremely irritable and aggressive, repeatedly getting into fights. The marked disregard for their own safety, as well as the safety of others, is also observed in reckless behavior such as speeding, driving under the influence, and engaging in sexual and substance abuse behavior that may put themselves at risk (APA, 2013).
Of course, the most known and devastating symptom of antisocial personality disorder is the lack of remorse for the consequences of their actions, regardless of how severe they may be (APA, 2013). Individuals often rationalize their actions at the fault of the victim, minimize the harmfulness of the consequences of their behaviors, or display indifference (APA, 2013). Overall, individuals with antisocial personality disorder have limited personal relationships due to their selfish desire and lack of moral conscious.
Borderline personality disorder. Individuals with borderline personality disorder display a pervasive pattern of instability in interpersonal relationships, self-image, affect, and instability (APA, 2013). The combination of these symptoms cause significant impairment in establishing and maintaining personal relationships. They will often go to great lengths to avoid real or imagined abandonment. Fears related to abandonment often lead to inappropriate anger as they often interpret the abandonment as a reflection of their own behaviors. It is not uncommon to experience intense fluctuations in mood, often observed as volatile interactions with family and friends (Herpertz & Bertsch, 2014). Those with borderline personality disorder may be friendly one day and hostile the next.
In efforts to prevent abandonment, individuals with borderline personality disorder will often engage in impulsive behaviors such as self-harm and suicidal behaviors. In fact, individuals with borderline personality disorder engage in more suicidal attempts and completion of suicide is higher among these individuals than the general public (Linehan et al., 2015). Other impulsive behaviors such as non-suicidal self-injury (cutting) and sexual promiscuity are often seen within this population, typically occurring during high stress periods (Sansone & Sansone, 2012).
Another key characteristic of borderline personality disorder is the unstable and/or intense relationships. For example, individuals may idealize or experience intense feelings for another person immediately after meeting them. Occasionally, hallucinations and delusions are present, particularly of a paranoid nature; however, these symptoms are often transient, and recognized as unacceptable by the individual (Sieswerda & Arntz, 2007).
Histrionic personality disorder. Histrionic personality disorder is the first personality disorder that addresses the pervasive and excessive need for emotion and attention from others. These individuals are often uncomfortable in social settings unless they are the center of attention. In efforts to gain the attention, the individual is often very lively and dramatic, using physical gestures and mannerisms along with grandiose language. These behaviors are initially very charming to their audience; however, they begin to wear due to the constant need for attention to be on them. If the theatrical nature does not gain the attention they desire, they may go to great lengths to gain the attention such as make-up a story or create a dramatic scene (APA, 2013).
To ensure they gain the attention they desire, individuals with histrionic personality disorder often dress and engage in sexually seductive or provocative ways. These sexually charged behaviors are not only directed at those in which they have a sexual or romantic interest, but to the general public as well (APA, 2013). They often spend significant amount of time on their physical appearance to gain the attention they desire.
Individuals with histrionic personality disorder are easily suggestable. Their opinions and feelings are influenced by not only their friends, but also by current fads (APA, 2013). They also have a tendency to over exaggerate relationships, considering casual acquaintanceships as more intimate in nature than they really are.
Narcissistic personality disorder. Similar to histrionic personality disorder, narcissistic personality disorder also centers around the individual; however, with narcissistic personality disorder, individuals display a pattern of grandiosity along with a lack of empathy for others (APA, 2013). The grandiose sense of self leads to an overvaluation of their abilities and accomplishments. They often come across as boastful and pretentious, repeatedly proclaiming their superior achievements. These proclamations may also be fantasized as a means to enhance their success or power. Oftentimes they identify themselves as “special” and will only interact with others of high status.
Given the grandiose sense of self, it is not surprising that individuals with narcissistic personality disorder need excessive admiration from others. While it appears that their self-esteem is extremely inflated, it is actually very fragile and dependent on how others perceive them (APA, 2013). Because of this, they may constantly seek out compliments and expect favorable treatment from others. When this sense of entitlement is not upheld, they can become irritated or angry that their needs are not met.
A lack of empathy is also displayed in individuals with narcissistic personality disorder as they often have difficulty (or choose not to) recognizing the desires or needs of others. This lack of empathy also leads to exploitation of interpersonal relationships, as they are unable to empathize other’s feelings (Marcoux et al., 2014). They often become envious of others who achieve greater success or possessions than them. Conversely, they believe everyone should be envious of their achievements, regardless of how small hey may actually be.
Avoidant personality disorder. Individuals with avoidant personality disorder display a pervasive pattern of social anxiety due to feelings of inadequacy and increased sensitivity to negative evaluations (APA, 2013). The fear of being rejected drives their reluctance to engage in social situations, in efforts to prevent others from evaluating them negatively. This fear extends so far that it prevents individuals from maintaining employment due to their intense fear of a negative evaluation or rejection.
Socially, they have very few if any friends, despite their desire to establish social relationships. They actively avoid social situations in which they can establish new friendships out of the fear of being disliked or ridiculed. Similarly, they are cautious of new activities or relationships as they often exaggerate the potential negative consequences and embarrassment that may occur; this is likely a result of their ongoing preoccupation of being criticized or rejected by others.
Despite their view as socially inept, unappealing, or inferior, individuals with avoidant personality disorder do not typically suffer from social skills deficits, but rather from misattributions of their own behaviors (APA, 2013).
Dependent personality disorder. Dependent personality disorder is characterized by pervasive and excessive need to be taken care of by others (APA, 2013). This intense need leads to submissive and clinging behaviors as they fear they will be abandoned or separated from their parent, spouse, or other person whom they are in a dependent relationship with. They are so dependent on this other individual that they cannot make even the smallest decisions without first consulting with them and gaining their approval or reassurance. They often allow others to assume complete responsibility of their life, making decisions in nearly all aspects of their lives. Rarely will they challenge these decisions as their fear of losing this relationship greatly outweighs their desire to express their own opinion. Should the relationship end, the individual experiences significant feelings of helplessness and quickly seeks out another relationship to replace the old one (APA, 2013).
When they are on their own, individuals with dependent personality disorder express difficulty initiating and engaging in tasks on their own. They lack self-confidence and feel helpless when they are left to care for themselves or engage in tasks on their own. In efforts to not have to engage in tasks alone, individuals will go to great lengths to seek out support of others, often volunteering for unpleasant tasks if it means they will get the reassurance they need (APA, 2013).
Obsessive-Compulsive personality disorder. OCPD is defined by an individual’s preoccupation with orderliness, perfectionism, and ability to control situations that they lose flexibility, openness, and efficiency in everyday life (APA, 2013). One’s preoccupation with details, rules, lists, orders, organizations or schedules overshadows the larger picture of the task or activity. In fact, the need to complete the task or activity is significantly impacted by the individuals self-imposed high standards and need to complete the task perfectly, that the task often does not get completed. The desire to complete the task perfectly often causes the individual to spend excessive amount of time on the task, occasionally repeating it until it is to their standard. Due to repetition and attention to fine detail, the individual often does not have time to engage in leisure activities or engage in social relationships. Despite the excessive amount of time spent on activities or tasks, individuals with OCPD will not seek help from others, as they are convinced that the others are incompetent and will not complete the task up to their standard.
Personally, individuals with OCD are rigid and stubborn, particularly with their morals, ethics, and values. Not only do they hold these standards for themselves, but they also expect others to have similar high standards, thus causing significant disruption to their social interactions. The rigid and stubborn behaviors are also seen in their financial status, as they are known to live significantly below their means, in order to prepare financially for a potential catastrophe (APA, 2013). Similarly, they may have difficulty discarding worn-out or worthless items, despite their lack of sentimental value.
While some argue that OCPD and OCD are one in the same, others argue that there is a distinct difference in that the personality disorder lacks definitive obsessions and compulsions (APA, 2013). Although many individuals are diagnosed with both OCD and OCPD, research indicates that individuals with OCPD are more likely to be diagnosed with major depression, generalized anxiety disorder, or substance abuse disorder than OCD (APA, 2013).
Vocabulary
- Personality Disorder: When personality traits result in significant distress, social impairment, and/or occupational impairment, they are considered to be a personality disorder.
- A pervasive pattern of disregard and violation of the rights of others. These behaviors may be aggressive or destructive and may involve breaking laws or rules, deceit or theft.
- Avoidant personality disorder. Individuals with avoidant personality disorder display a pervasive pattern of social anxiety due to feelings of inadequacy and increased sensitivity to negative evaluations (APA, 2013).
- Borderline Personality Disorder
- A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity.
Dialectical behavior therapy is a form of cognitive-behavior therapy that draws on principles from Zen Buddhism, dialectical philosophy, and behavioral science. It started out as a treatment for Borderline Personality disorder but has become a general treatment for self-regulation difficulties.
- Narcissistic Personality Disorder
- A pervasive pattern of grandiosity (in fantasy or behavior), need for admiration, and lack of empathy.
Schizoid Personality Disorder: Individuals with schizoid personality disorder display a persistent pattern of avoidance from social relationships along with a limited range of emotion among social relationships.
Histrionic personality disorder. Histrionic personality disorder is the first personality disorder that addresses the pervasive and excessive need for emotion and attention from others.
Dependent personality disorder is characterized by pervasive and excessive need to be taken care of by others.
Obsessive-Compulsive personality disorder. OCPD is defined by an individual’s preoccupation with orderliness, perfectionism, and ability to control situations that they lose flexibility, openness, and efficiency in everyday life (APA, 2013).
References
- Allik, J. (2005). Personality dimensions across cultures. Journal of Personality Disorders, 19, 212–232.
- American Psychiatric Association (2012). Rationale for the proposed changes to the personality disorders classification in DSM-5. Retrieved from http://www.dsm5.org/ProposedRevision/Pages/PersonalityDisorders.aspx.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association.
- American Psychiatric Association. (2001). Practice guidelines for the treatment of patients with borderline personality disorder. Washington, DC: Author.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.) Washington, D.C: American Psychiatric Association.
- Bateman, A. W., & Fonagy, P. (2012). Mentalization-based treatment of borderline personality disorder. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 767–784). New York, NY: Oxford University Press.
- Beck, A. T., Freeman, A., Davis, D., and Associates (1990). Cognitive therapy of personality disorders, (2nd ed.). New York, NY: Guilford Press.
- Bornstein, R. F. (2012). Illuminating a neglected clinical issue: Societal costs of interpersonal dependency and dependent personality disorder. Journal of Clinical Psychology, 68, 766–781.
- Caspi, A., Roberts, B. W., & Shiner, R. L. (2005). Personality development: Stability and change. Annual Review of Psychology, 56, 453–484.
- DeYoung, C. G., Hirsh, J. B., Shane, M. S., Papademetris, X., Rajeevan, N., & Gray, J. (2010). Testing predictions from personality neuroscience: Brain structure and the Big Five. Psychological Science, 21, 820–828.
- Gunderson, J. G. (2010). Commentary on “Personality traits and the classification of mental disorders: Toward a more complete integration in DSM-5 and an empirical model of psychopathology.” Personality Disorders: Theory, Research, and Treatment, 1, 119–122.
- Gunderson, J. G., & Gabbard, G. O. (Eds.), (2000). Psychotherapy for personality disorders. Washington, DC: American Psychiatric Press.
- Hare, R. D., Neumann, C. S., & Widiger, T. A. (2012). Psychopathy. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 478–504). New York, NY: Oxford University Press.
- Hooley, J. M., Cole, S. H., & Gironde, S. (2012). Borderline personality disorder. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 409–436). New York, NY: Oxford University Press.
- Hopwood, C. J. (2011). Personality traits in the DSM-5. Journal of Personality Assessment, 93, 398–405.
- John, O. P., Naumann, L. P., & Soto, C. J. (2008). Paradigm shift to the integrative Big Five trait taxonomy: History, measurement, and conceptual issues. In O. P. John, R. R. Robins, & L. A. Pervin (Eds.), Handbook of personality. Theory and research (3rd ed., pp. 114–158). New York, NY: Guilford Press.
- John, O. P., Robins, R. W., & Pervin, L. A. (Eds.), (2008). Handbook of personality. Theory and Research (3rd ed.). New York, NY: Guilford Press.
- Livesley, W. J. (2011). Confusion and incoherence in the classification of personality disorder: Commentary on the preliminary proposals for DSM-5. Psychological Injury and Law, 3, 304–313.
- Lynam, D. R., & Widiger, T. A. (2001). Using the five factor model to represent the DSM-IV personality disorders: An expert consensus approach. Journal of Abnormal Psychology, 110, 401–412.
- Lynch, T. R., & Cuper, P. F. (2012). Dialectical behavior therapy of borderline and other personality disorders. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 785–793). New York, NY: Oxford University Press.
- Miller, J. D., Widiger, T. A., & Campbell, W. K. (2010). Narcissistic personality disorder and the DSM-V. Journal of Abnormal Psychology, 119, 640–649.
- Millon, T. (2011). Disorders of personality. Introducing a DSM/ICD spectrum from normal to abnormal (3rd ed.). New York, NY: John Wiley & Sons.
- Mullins-Sweatt; Bernstein; Widiger. Retention or deletion of personality disorder diagnoses for DSM-5: an expert consensus approach. Journal of personality disorders 2012;26(5):689-703.
- Perry, J. C., & Bond, M. (2000). Empirical studies of psychotherapy for personality disorders. In J. Gunderson and G. Gabbard (Eds.), Psychotherapy for personality disorders (pp. 1–31). Washington DC: American Psychiatric Press.
- Roberts, B. W., & DelVecchio, W. F. (2000). The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin, 126, 3–25.
- Shedler, J., Beck, A., Fonagy, P., Gabbard, G. O., Gunderson, J. G., Kernberg, O., … Westen, D. (2010). Personality disorders in DSM-5. American Journal of Psychiatry, 167, 1027–1028.
- Skodol, A. (2012). Personality disorders in DSM-5. Annual Review of Clinical Psychology, 8, 317–344.
- Smith, G. G., & Zapolski, T. C. B. (2009). Construct validation of personality measures. In J. N. Butcher (Ed.), The Oxford Handbook of Personality Assessment (pp. 81–98). New York, NY: Oxford University Press.
- Torgerson, S. (2012). Epidemiology. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 186–205). New York, NY: Oxford University Press.
- Widiger, T. A. (2009). Neuroticism. In M. R. Leary and R.H. Hoyle (Eds.), Handbook of individual differences in social behavior (pp. 129–146). New York, NY: Guilford Press.
- Widiger, T. A., & Trull, T. J. (2007). Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist, 62, 71–83.
- Yamagata, S., Suzuki, A., Ando, J., One, Y., Kijima, N., Yoshimura, K., … Jang, K. L. (2006). Is the genetic structure of human personality universal? A cross-cultural twin study from North America, Europe, and Asia. Journal of Personality and Social Psychology, 90, 987–998.